Impact of Passing Through Negotiated Rebates on Oral Antidiabetic Drugs (OAD) Adherence
-
Diabetes affects nearly 10 million commercially insured patients in the US and poses significant human and economic risks to those patients and society
-
Sharing manufacturer rebates for brand OADs directly with commercially insured patients can reduce their net drug out-of-pocket spending
-
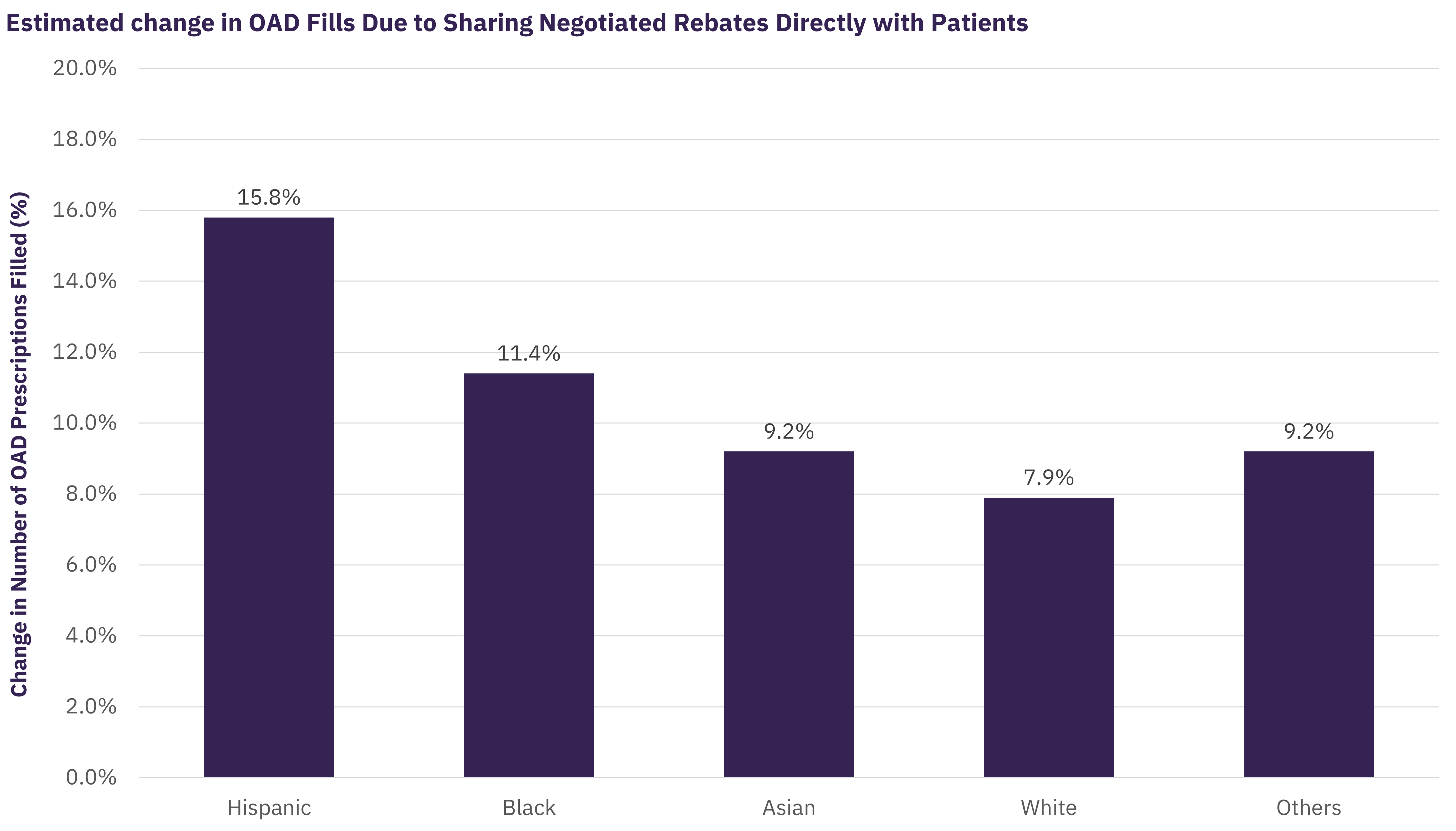
GlobalData estimates that communities of colour can expect the greatest improvements in adherence since diabetes is known to present a substantial health and economic burden to them
Impact of Passing Through Negotiated Rebates on Oral Antidiabetic Drugs (OAD) Adherence
The Centers for Disease Control and Prevention estimates that 13% of all the US adults have diabetes, and even more meet criteria for prediabetes. Aside from its pervasive nature, it is known that diabetes presents a substantial health and economic burden that disproportionately affects Black, Native American/Alaskan Native, and Hispanic populations. A study commissioned by the American Diabetes Association reports that diagnosed diabetes cost the nation $327 billion in 2017, including $237 billion in direct medical costs and $90 billion in reduced productivity. The study also noted that there are differences in diabetes-related health expenditures across race and ethnicity groups; for example, Black patients with diabetes incur 7% higher diabetes-attributed healthcare expenditures on average compared to white patients. Disparities in diabetes outcomes arise, in great part, from the inequities in the healthcare system, which can be exemplified and exacerbated through inequitable access to essential diabetes medications. Extensive evidence links better medicine adherence to reduced diabetes complications, lower medical spending, and lower mortality.
High out-of-pocket (OOP) costs for diabetes medicines are key barriers to taking prescribed medicines that can reduce risk of diabetes complications, hospitalization and emergency visits, and associated healthcare costs. One option to reduce patient out-of-pocket costs is to restructure how health plans share negotiated rebates, discounts, and other payments received from pharmaceutical manufacturers with insured patients. Sharing negotiated rebates directly with patients would substantially reduce patient out-of-pocket costs, while also alleviating a major barrier affecting access to medicines for disadvantaged populations.
Research shows that patient use of healthcare services decreases when faced with higher OOP costs. In the case of prescription medicines, a 10% increase in OOP costs is associated with a 1-3% decrease in the number of prescriptions filled. GlobalData analysis estimates that cost sharing savings from passing through 100% of rebates at the pharmacy would increase the number of OAD prescriptions filled among the commercially insured population by 9.2% on average. Literature also suggests that demand sensitivity to OOP costs for prescription medicines is influenced by race/ethnicity and insurance type. GlobalData’s report on “The Impact of Sharing Manufacturer Rebates for Oral Anti-Diabetic Medications at the Point of Sale with Patients in the Commercial Market” finds that expected improvements in adherence due to reduced cost sharing from passing through negotiated rebates is particularly high among Black and Hispanic enrollees. For example, the estimated impact of sharing rebates with Hispanic patients (15.8% increase) is twice that of white patients (7.9% increase).
Related Data & Insights
Related Companies
United States of America
United States of America
China
Switzerland
United States of America
United States of America
United States of America
United States of America
Germany
France
Don’t wait - discover a universe of connected data & insights with your next search. Browse over 28M data points across 22 industries.
Access more premium companies when you subscribe to Explorer
Get in touch about GlobalData Company reports
Contact the team or request a demo to find out how our data can drive your business forward